Andrigolitis is an illness that frequently appears in recent discussions about health matters, often due to a lack of broader knowledge, it is highly misinterpreted. Early awareness of andrigolitus aids in effective management of symptoms and treatment choices. Better understanding allows individuals to better navigate this condition.
Let us go through this step by step.
What Is Andrigolitis?
Andrigolitis is the chronic inflammatory condition that affects soft tissues and joints in a person. It is not well recognized, but has similarities with autoimmune diseases. The variability of symptoms among patients complicates diagnosis and is unique to many-andrigolitis.
While the exact cause of this condition is still elusive, a combination of inheritance, surroundings and the body’s natural defense mechanisms is believed to be the cause. Most importantly, timely identification aids in reducing the burden of chronic complications.
Most Common Symptoms To Pay Attention To
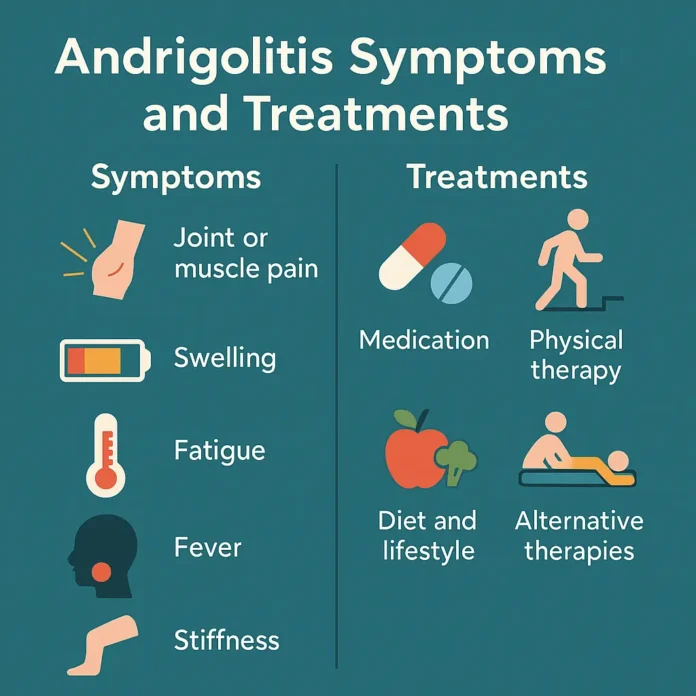
Patients have a higher likelihood of managing andrigolitis if the condition is recognized and managed early. Here are some of the most frequently reported symptoms:
- Chronic pain in muscles or joints
- Swelling in the areas of concern
- Persistent fatigue
- Mild fever or chills
- Subtle rashes
- Reduced mobility after long periods of stillness
- Mild to moderate skin rashes
- Mild to moderate skin rashes
While some of these symptoms may be intermittent, patients find that they often worsen during exacerbations. Many people experience early symptoms and signs which, if ignored, can lead to considerably more severe pain or movement restriction later in life.
How Doctors Diagnose It
The process of evaluating a patient for andrigolitis is multi-step. The condition’s overlapping symptoms with other diseases makes andrigolitis particularly challenging to diagnose; as such, clinical examinations alongside the patient’s history and laboratory investigations are required. In most cases, patients undergo
- Laboratory investigation specialized for detecting inflammation markers
- MRI and ultrasound imaging of soft tissues
- Symptom journals spanning several weeks
And in some instances, directly looking at the affected tissues via biopsy. The goal is to obtain an accurate diagnosis and rule out the presence of other, similar conditions.
Efficient Treatment Approaches
Fortunately, there are multiple options to try in treating andrigolitis. Each strategy is tailored to the individual patient’s needs, but typical methods include:
1. Medication Management
To alleviate pain and swelling, some inflammation medications may be prescribed. For more extreme cases of andrigolitis, other pharmacological treatment methods such as immunosuppressive drugs and/or corticosteroids may be suggested. These medications help control the body’s immunological processes and reduce the chances of flare-up.
2. Physical Therapy
Concentrated movement therapy maintains joint range of motion and assists with active mobility. Because physical therapists often devise routines based on personal requirements, this approach is both efficient and beneficial.
3. Dietary and Lifestyle Changes
Following an anti-inflammatory diet can bolster general wellness. Patients should focus on good sources of omega 3 fatty acids, green leafy vegetables, and whole grains. In addition to resting, staying active, and reducing stress can significantly improve overall health.
4. Other Treatment Suggestions
Some patients utilize acupuncture, massage, or herbal supplements to help soothe their symptoms. Though these therapies should not replace standard medical treatment, they can be safely incorporated into balanced care when used prudently alongside other treatments.
Managing Andrigolitis Day to Day
Pragmatic approaches to living with andrigolitis, require structure and consistency. Symptom journaling makes it easier for the patient and the doctor to notice patterns. With gentle yoga and ergonomic office furniture, investing in comfort aids can greatly enhance mobility and overall wellness.
Both online and offline support groups provide emotional assistance. Sharing struggles fosters resilience and counters a sense of isolation.
When To See A Specialist
It is best to consult a specialist if symptoms persist for several weeks or begin interfering with daily activities. Specialists in complex inflammatory conditions, like andrigolitis, are particularly rheumatologists.
Comfort is enhanced and the risk of permanent tissue damage is reduced with early intervention. Thus, medical intervention should not be postponed when symptoms worsen.
FAQs About andrigolitis
Q1: Is andrigolitis a permanent condition?
Not and entirely. Some people do describe it as chronic, but for others, symptoms are treated, and with active management, lifestyle modifications, symptoms can improve.
Q2: Can diet affect andrigolitis symptoms?
Yes, symptoms and general wellbeing can be improved by skincare anti-inflammatory diets.
Q3: Is andrigolitis contagious?
No, it is non-contagious. It is thought to be triggered by endogenous phenomena such as immune responses or a genetic predisposition.
Q4: Can children develop andrigolitis?
While it is more common in adults, a few cases have been documented in younger teenagers. In young children, seeing a specialist is very important.
Q5: Are there any long-term complications?
If left unmanaged, andrigolitis could cause dermal or joint tissue damage. However, with appropriate treatment, this risk can be minimized considerably.